The toxic drug crisis in British Columbia is reshaping the province’s approach to addictions and public health.
The province declared the toxic drug crisis a public health emergency in 2016. As the crisis continues, the impact is felt differently in various regions, highlighting the need for tailored responses and increased awareness in addressing unique place-based challenges.
For context, it is important to understand how the toxic drug crisis is affecting British Columbia as a whole. The BC Coroners Service provides reporting on deaths associated with toxic drugs. BC recorded 2,551 deaths from toxic drug use in 2023, a 7 percent increase from 2022 (2,385 deaths). Across the province in 2023, 78 percent of those who died were male. Of the total deaths, most occurred in individuals aged 30-39 (25 percent), followed by 50-59 (23 percent) and 40-49 (22 percent). The most common mode of consumption identified in 2023 drug deaths was smoking (65 percent), and the drug most involved in drug toxicity deaths was fentanyl and its analogues (found in 85 percent of deaths). This was followed by methamphetamine and amphetamine (found in 50 percent of deaths) and benzodiazepines (found in 43 percent of deaths).
What do the numbers say about the toxic drug crisis in the Columbia Basin-Boundary Region?
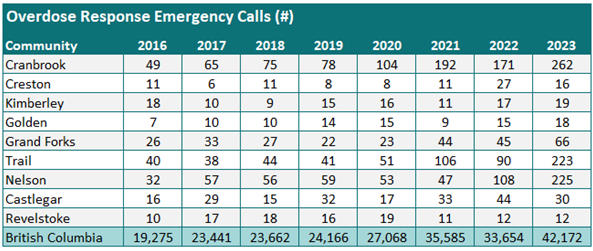
Illicit drug toxicity deaths are reported at the Local Health Area (LHA) level. The table below displays the drug toxicity death rate per 100,000 persons by LHA between 2016 and 2023. This allows for comparison between regions with different population sizes. The total number of deaths in 2023 is also included to see the number of lives lost in each community.
In 2023, the Cranbrook LHA had the highest rate of illicit drug toxicity deaths at 67.7 deaths per 100,000 persons (20 deaths). Following this was the Grand Forks LHA with a rate of 62.7 deaths per 100,000 persons (6 deaths), the Nelson LHA with a rate of 57.0 deaths per 100,000 persons (16 deaths), and the Trail LHA with a rate of 51.0 deaths per 100,000 persons (11 deaths). In these four LHAs, the rate of deaths exceeds the provincial rate of 46.2 deaths per 100,000 persons.
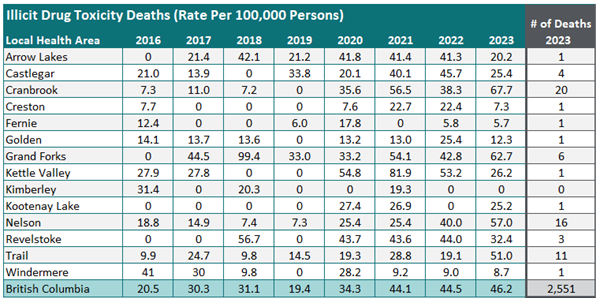
Overdose Response Emergency Calls
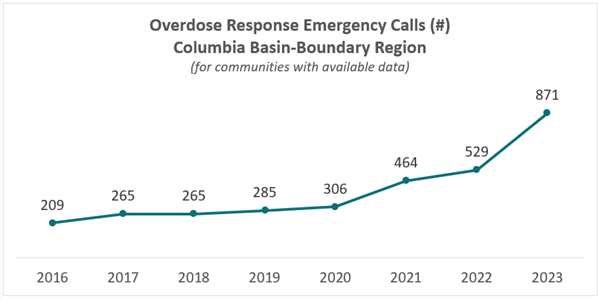
Another available dataset that sheds light on the toxic drug crisis is the volume of overdose emergency calls paramedics respond to in each community. As shown in the figures below, in addition to an increase in drug toxicity deaths, there is also an increase in emergency calls for overdose response, underscoring the escalating impact of the crisis. BC Emergency Health Services reported a provincial total of 42,172 events for overdose responses in 2023. Of the nine communities in the Columbia Basin-Boundary Region with available data, the communities with the most calls include Cranbrook (262), Nelson (225), and Trail (223). Between 2016 and 2023, the number of overdose response calls for communities in the region with available data went up 317 percent, from a combined total of 209 in 2016 to 871 in 2023.
Using Data for Evidence-Based Responses
The impacts of the toxic drug crisis differ between urban and rural areas. As reported by the Office of the Auditor General of British Columbia, rural communities experience gaps in health equity and barriers when attempting to access appropriate supports. Substance use and emergency responses to overdose are often more noticeable in smaller communities, potentially exacerbating stigma, which, in turn, further contributes to health inequities. Understanding localized data on the toxic drug crisis is important for evidence-based decision-making and developing targeted strategies and interventions that address the region’s specific needs and challenges.
Article supplied by Selkirk College: Selkirk Innovates
Be the first to know! Don’t miss out on breaking news and daily updates in your area. Sign up to MyNelsonNow News Alerts.